Aug. 30, 2013 Research Highlight Medicine / Disease
Drug treatment improves survival of insulin-producing cells
Pretreatment with a calcium-blocking drug improves the effectiveness of islet transplantation for diabetes in mice
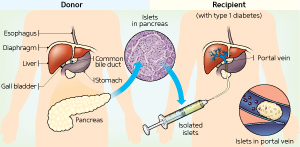 Figure 1: The process of clinical islet transplantation. Reproduced from PLoS Medicine 1, e58 (2004). Licensed under CC by 2.5. © 2004 M. A. Naftanel and D. M. Harlan
Figure 1: The process of clinical islet transplantation. Reproduced from PLoS Medicine 1, e58 (2004). Licensed under CC by 2.5. © 2004 M. A. Naftanel and D. M. Harlan
The transplantation of insulin-producing islet cells from a donor pancreas could help diabetes sufferers avoid the need for daily insulin injections. However, the use of this experimental procedure is hampered by an immune response in the recipient that often rejects the transplanted islet cells. Masaru Taniguchi from the Laboratory for Immune Regulation at the RIKEN Center for Integrative Medical Sciences and Yohichi Yasunami from Fukuoka University have now led research that has improved the efficiency of the procedure by pretreating the islet cells with a drug that blocks the sodium-calcium exchanger (NCX) protein1.
Islet transplantation often involves the use of islet cells from two or three different donors in order to achieve sufficient cell engraftment. “This low efficiency has been a major obstacle facing clinical islet transplantation,” says Taniguchi.
Taniguchi, Yasunami and their respective lab groups set out to improve the islet transplantation procedure by pretreating islet cells prior to transplantation with a drug that blocks the NCX protein. This pretreatment protected the cells from innate immune responses in the liver, the site of islet transplantation, which led to longer-term survival of the cells in mouse models of diabetes.
“Pretreatment of donor islets with an NCX inhibitor prior to transplantation prevents early loss of transplanted islets and affords a new strategy to improve the efficiency of islet transplantation,” says Taniguchi. Notably, the method allows for improved engraftment efficiencies without requiring transplant recipients to take any additional anti-rejection drugs. “Our new strategy to target donor islets does not add further risks to recipients,” notes Taniguchi.
The drug pretreatment is thought to work by stopping NCX from boosting the intracellular levels of calcium ions. Normally, this calcium influx leads to low oxygen conditions, which trigger the release of a protein called high-mobility group box 1 (HMGB1) from islets soon after their transplantation. HMGB1 in turn activates immune cells, causing the early loss of transplanted islets. The NCX-blocking drug, called SEA0400, can prevent this cascade of events.
After transplanting pretreated and untreated islets into diabetic mice, the research team found that mice receiving SEA0400-treated islets displayed normal blood sugar control. In contrast, the control animals, which received the same number of untreated islets, experienced elevated blood sugar levels due to a lack of functional insulin-producing cells, which presumably had been attacked by the immune system. This same effect was seen whether the transplanted islets were human or murine in origin.
References
- 1. Mera, T., Itoh, T., Kita, S., Kodama, S., Kojima, D., Nishinakamura, H., Okamoto, K., Ohkura, M., Nakai, J., Iyoda, T. et al. Pretreatment of donor islets with the Na+/Ca2+ exchanger inhibitor improves the efficiency of islet transplantation. American Journal of Transplantation advance online publication, 7 June 2013. doi: 10.1111/ajt.12306
