Apr. 17, 2015 Research Highlight Biology
An infectious imprint on liver cancer
Cases of liver cancer caused by chronic hepatitis share a common mutational profile
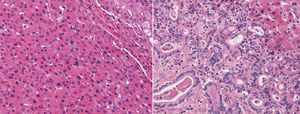 Figure 1: Microscopy images of liver tumor tissue from the two main forms of liver cancer: hepatocellular carcinoma (left) and biliary liver cancer (right). The two types of cancer display distinct gene activity profiles that vary between patients with and without hepatitis. Reprinted by permission from Macmillan Publishers Ltd: Nature Communications (Ref. 1), copyright (2015)
Figure 1: Microscopy images of liver tumor tissue from the two main forms of liver cancer: hepatocellular carcinoma (left) and biliary liver cancer (right). The two types of cancer display distinct gene activity profiles that vary between patients with and without hepatitis. Reprinted by permission from Macmillan Publishers Ltd: Nature Communications (Ref. 1), copyright (2015)
People with liver cancer who are chronically infected with hepatitis share genetic mutations not found in liver cancer patients without the virus1. This RIKEN-led discovery could help doctors tailor treatments for liver cancer—the third leading cause of cancer death worldwide.
Liver cancer kills more than half a million people globally each year. Although the disease comes in a number of different forms, around 90 per cent of cases are classified as hepatocellular carcinoma (HCC), a type of cancer that begins in liver cells. Most of the remaining 10 per cent of tumors arise on the bile ducts that enter the liver. This type of biliary liver cancer is generally more aggressive than HCC, and typically has a much worse prognosis (Fig. 1).
To better understand the molecular differences between these two forms of liver cancer, a large collaborative team of researchers led by Hidewaki Nakagawa from the Laboratory for Genome Sequencing Analysis at the RIKEN Center for Integrative Medical Sciences sequenced the genomes of 30 biliary and 60 HCC tumors from patients with and without hepatitis viral infections—a major risk factor for all types of liver cancer. The team also studied gene expression patterns by examining RNA sequencing data from a subset of the cancers.
The team found that gene activity profiles largely tracked the cancer subtype, with biliary tumors expressing one suite of genes and HCC tumors another. However, Nakagawa and his co-workers also found that the mutational profiles were well matched with infection status. Tumors that arose in people with chronic hepatitis infections showed one pattern of DNA substitutions, whereas samples from liver cancer patients without the virus displayed a different pattern.
“Our results suggest that hepatitis can cause mutations,” says Akihiro Fujimoto, a senior research scientist at RIKEN and lead author of the study. This same kind of clustering according to an external factor is also seen in other types of cancers with environmental triggers, such as melanoma skin cancer, which is often caused by ultraviolet sunlight, and lung cancer, which often results from smoking tobacco.
In the biliary liver tumors, the researchers found 32 genes that were repeatedly mutated in different samples. A search for these mutations in an independent dataset of 68 tumors from biliary liver cancer patients confirmed the presence of many altered genes, including genes involved in cell structure, chromosome maintenance, tumor suppression and cancer promotion. Several of these genes now provide promising leads for future drug development.
References
- 1. Fujimoto, A., Furuta, M., Shiraishi, Y., Gotoh, K., Kawakami, Y., Arihiro, K., Nakamura, T., Ueno, M., Ariizumi, S-i., Nguyen, H. H. et al. Whole-genome mutational landscape of liver cancers displaying biliary phenotype reveals hepatitis impact and molecular diversity. Nature Communications 6, 6120 (2015). doi: 10.1038/ncomms7120
